ST. GEORGE — The Utah Department of Health has released a report showing unique health disparities between legislative districts in the state.
Health disparities are defined as health outcomes that are “avoidable, unfair and unjust,” according to the Utah Health Department. They are closely linked with social determinants of health factors, such as a person or community’s access to things like transportation, housing, clean air and proximity to health care, all of which affect health outcomes.
“Where you live, basically, can decide what your health is going to be like,” said Courtney Bullard, education and collaborations director at Utah Health Policy Project.
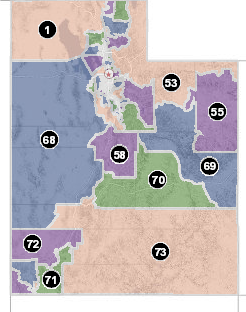
While health rankings are often determined by looking at states, cities or counties, this research breaks it down by legislative district and narrows it down even further by “Utah Small Areas” within those districts.
Most of the Utah Small Areas within the districts are designated by towns, and each is between 8,000 to 86,000 in population.
The health department looked at a number of factors identified in the Utah Health Improvement Index (HII) that could be considered either a health disparity or an adverse health outcome.
All health disparities are considered adverse health outcomes, but not all adverse health outcomes are health disparities. Health disparities only exist if there is a preventable factor contributing to the poor health outcome.
“They are all over the state. Especially in rural areas, where those populations are affected in different ways than urban areas with health,” Bullard said.
The HII consists of nine indicators based on demographics, socioeconomic deprivation, economic inequality, resource availability and opportunity structure. Locations are ranked from “very low” to “very high” on the HII, with higher groups needing the most improvements.
Health disparities are determined if a Utah Small Area with a poor health outcome has a high HII ranking compared to the state average, and an adverse health outcome exists if the area with the poor health outcome has a low or average HII.
Statewide, 1 in 3 senate districts and 1 in 4 house districts experienced six or more health discrepancies.
The study compared the rates of diabetes, obesity, poor mental health, smoking, suicide, drug poisoning, infant mortality, life expectancy, having no health insurance and those reporting having poor or fair general health.
Cedar City has the highest number of discrepancies in Southern Utah, fitting into the “very high” category of HII.
The discrepancies in Cedar City include the number of adults reporting poor mental health was found to be 4.9% higher than the state average of 16.5%, and their life expectancy averages at 78.6 years, while the state average is 79.8.
Rural areas of Washington County were also among the “very high” HII group, with a discrepancy of the percent of people without health care coverage being over twice as much as Utah’s average of 10%.
In fact, all of the Utah Small Areas in Utah legislative districts 71 and 75 had a higher than average percentage of people without health insurance. This may be because a larger number of people living in rural communities work in agriculture and are self-employed, meaning they are less likely to have health insurance, Southwest Utah Public Health Department spokesperson Dave Heaton said.
While the Utah Small Area consisting of Hurricane and LaVerkin did not have any health discrepancies, it was ranked as “high” in the HII due to a higher infant mortality rate, a higher number of smokers and more adults reporting having poor mental health.
St. George and Washington City both ranked “average” on the HII scale, with no health discrepancies. They both had an adverse health outcome for the number of suicides, which were above the average number of suicides per 100,000 people statewide.
The Ivins/Santa Clara small area was the only one to rank “low” on the HII scale.

The reason these disparities exist largely has to do with social determinants of health, or non-health related factors that affect a person’s health outcomes, such as housing instability, utility needs, food insecurity, interpersonal violence and transportation.
While the study released by the Utah Department of Health does not list the determinants that affect the disparities they found, their data does give local health officials and legislators the tools to find them on their own.
Breaking health disparities down by legislative district makes it even easier for Utah legislators to see exactly what health disparities are happening in their districts, determine which social determinants of health are causing them and what they can do to prevent them.
“These are things in this report that can be changed, that can be stopped through targeted policies,” Bullard said. “And that’s what we really wanted to encourage legislators to do with this wealth of research, is they can now look in their district and they can isolate problems that are negatively impacting their constituents.”
Utah State Rep. Brad Last said studies like these help lawmakers make informed decisions about what legislation is needed to benefit the people in their districts.
“As legislators, we try to make decisions based on data, so I think that kind of information is good. And if there are areas of the state that are having problems, then I think that is an indication of areas where we should put more effort,” he said.
Many of the social determinants of health, however, are more specific to individuals than to the community as a whole, making them difficult to address, Health Department Director Dr. David Blodgett said.
“When you start talking about social determinants of health, it’s not a standard number for everybody … Quantifying and trying to figure out how to create programs to deal with that is lagging because it’s so unique to the individual. And it doesn’t lend itself to needs that are kind of societal,” he said.
One major community factor in Southern Utah, however, is a lack of housing availability, and more specifically, affordable housing availability.
There are things being done statewide to address the social determinants of health. The Utah Health Policy Project is currently working to encourage the expansion of Medicaid to make health insurance, and therefore health care, available to more people, Bullard said.
Blodgett said the Intergenerational Poverty Initiative is another effort to help break the cycle of multigenerational poverty.
Even though many of these health discrepancies and social determinants of health have been determined, there is a lack of funding and resources allotted to addressing them.
“I think there is a greater awareness of the problems than ever has been, but as far as have we started to get the resources focused in the right direction, I don’t think so,” Blodgett said.
The full report of health discrepancies in every Utah legislative district can be found online.
Copyright St. George News, SaintGeorgeUtah.com LLC, 2019, all rights reserved.